Why IBS Symptoms May Be Worse During Your Period
Have you noticed that IBS symptoms seem to ramp up in the days leading up to your period? Or that your poop gets a bit weird during your period?
You’re not alone!
This is a concern I hear from many of my clients, and have actually experienced myself… and there’s a clear reason why this happens.
It all starts with hormones
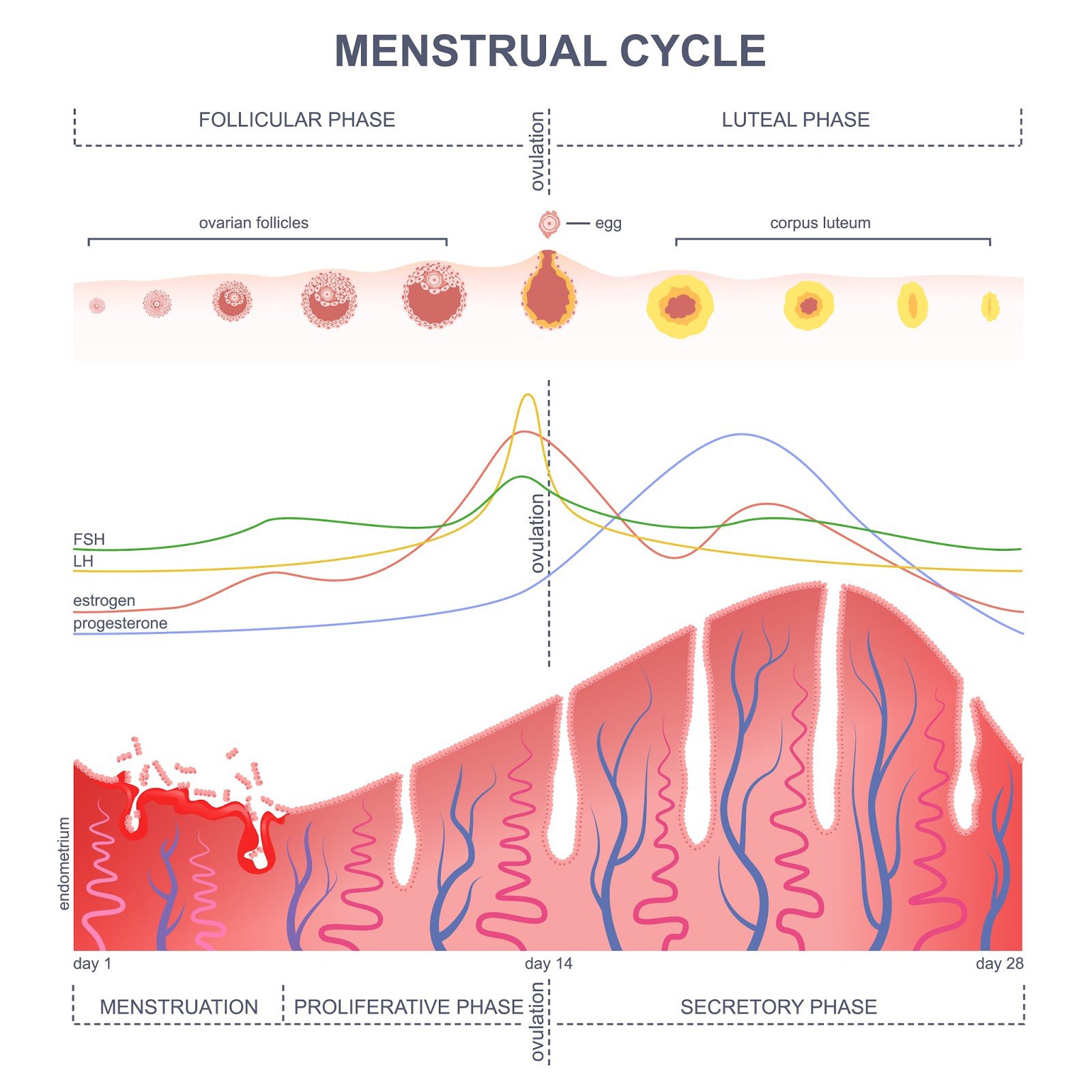
There are 2 major hormones involved in menstruation: estrogen and progesterone. These hormones are not only at work in our sex organs, but also have receptors in the gastrointestinal tract… meaning that fluctuations in both hormones can influence gut function and IBS symptoms.
Before ovulation, estrogen levels reach their peak, then rapidly drop at the end of ovulation. This shift in estrogen can increase symptoms of bloating and constipation.
During the luteal phase (before your period), progesterone levels reach their peak, then drop at the start of menstruation (your period). This can increase symptoms of abdominal pain, bloating, diarrhea, and nausea.
What’s your poop personality? Find out here!
What about period poops?
When you are menstruating (aka on your period), there are fatty acids called prostaglandins that are released to help relax the muscle tissues in the uterus to help with the shedding of the uterine lining.
Prostaglandins also increase in muscle tissues in the gut, which leads to relaxation and increased stool output. This can cause loose stools and urgency, otherwise known as “period poops.”
When you pack on period poops following days of constipation, these symptoms may feel more severe. For those with IBS, visceral hypersensitivity can also explain why the constipation, as well as the period poops contribute to more pain, which can be tough to differentiate from period-related pain.
How does IBS affect periods?
On the opposite side of the table, studies show that having IBS can also increase your risk or severity of period symptoms, including painful cramps, backache, fatigue, insomnia, food sensitivity, and water retention.
Mood-related changes during menstruation (PMS) is not shown to increase for those with IBS. However, anxiety related to the increase in digestive symptoms during this time may increase, which can then impact mood.
Why in the world is all of this connected? We don’t fully understand the cause. There’s a lot of research to be done, so hopefully we have more answers in the coming years.
And what about those with PCOS and endometriosis?
PCOS and endometriosis are two common gynecological disorders, that are both related to the balance of female sex hormones and the function of reproductive organs.
Studies show a connection between IBS and these disorders, but again there’s a lot we don’t fully understand. Symptoms can overlap between either of these and IBS, and many women will carry diagnoses for both.
We aren’t sure which disorder causes or worsens the other, or if there’s an issue with misdiagnosing one for the other, but we do know that it’s important to develop a plan to address the common issues in both to manage symptoms fully. If endometriosis is present, there is also a chance that this can grow on bowel tissues, so this may also be explored during diagnosis.
So…. what do you do from this information?
If you’re dealing with an increase in IBS symptoms after ovulation or in the days leading up to your period, there are a few things you can do to support your body and help improve your symptoms.
Know your cycle. Tracking your cycle will allow you to know when you are ovulating, in the luteal phase, and approaching menstruation. Being proactive is key to preventing symptoms, so that starts with knowing your body. You can use apps, basal temperature thermometers, and more to do this. Chat with your gynecologist if you need guidance.
Support your gut with gentle exercise, adequate hydration and fiber, reduction in trigger foods, and plenty of sleep leading up to the days when you experience symptoms the most. Avoid large amounts (doesn’t mean exclude completely!) of trigger foods during that time. Giving your body a little extra care will help prevent the symptoms from coming on in the first place.
Prioritize self care and stress management, daily. This can include morning sunshine, movement, exercise, nervous system regulation, boundaries, and quality sleep. Stress can impact your hormones and lead to more PMS systems, as well as irregular cycles. Stress can also cause more IBS symptoms, which combined can be tough to manage.
Ease symptoms you are not able to fully prevent with gentle movement (like yoga!), peppermint oil or capsules, ginger tea, heating pads, warm baths, and warm non-trigger foods!
If you need personalized support for your cycle and your IBS, our team at Gutivate may be able to help. Schedule a consult call here to see if it’s the right fit for you.
Sources:
https://www.monashfodmap.com/blog/ibs-and-that-time-of-month/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527267/
https://gut.bmj.com/content/50/4/471
https://www.monashfodmap.com/blog/ibs-and-that-time-of-month/
Are you frustrated with your IBS symptoms? Do you desire to be confident in your food choices? Do you want to have a healthier relationship with your body and diet? Are you ready to take control of your IBS?