What causes GERD and reflux?
Do you experience reflux and heartburn? Have you been diagnosed with GERD?
If so, you may be wondering how this happened. Unfortunately when you get a diagnosis, there’s not a lot of time available to talk through the full picture, and treatment will often be recommended before you understand what actually went wrong.
If any of that is you, you’re in the right place. This article will break down what causes GERD so that you can better understand your own body. Before we get started, it may help for you to think back over your health history and when symptoms began for you. Write down everything that comes to mind during that time of your life and then keep that in mind as you read this article to find the connections that may be at play for you.
What happens when you eat or drink?
We can’t dive into GERD without first reviewing what happens when you eat a meal or drink something, and then where in that process things start to get disconnected.
Digestion, and your digestive tract, starts with your oral cavity, which includes your mouth (lips, teeth, and tongue) and pharynx (aka your throat). Your oral cavity has 4 main jobs with digestion: mechanical breakdown of food through chewing, chemical breakdown through the release of salivary amylase (enzyme that breaks down carbohydrates), sensory processing to signal the rest of your digestive tract to “turn on,” and lubrication of food with saliva to make it easier to move through the pharynx and esophagus.
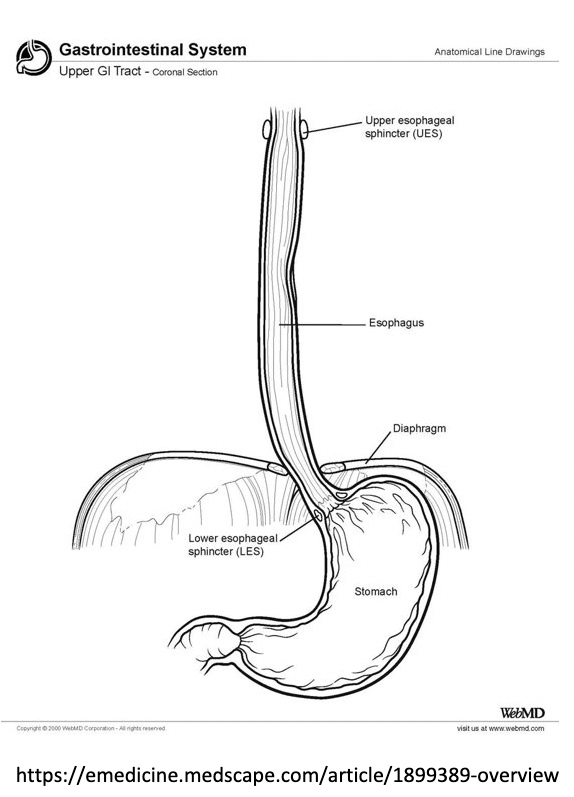
Once food leaves your pharynx, it passes through the upper esophageal sphincter (think of this like a circular door that opens for food and then stays closed the rest of the time) into the esophagus. Your esophagus is made up of both skeletal and smooth muscle that move food through contractions and relaxations, called peristalsis.
Once food gets to the end of the esophagus, it passes through the lower esophageal sphincter (LES) into the stomach. This is an important part of the process when it comes to GERD, because this is the “door” that separates what should stay in the stomach (food, acid, bile) from the esophagus.
See the image to the right to put this together as a visual and compare to your own body.
Now that food is in your stomach, there 2 major phases of digestion that happen there: mechanical and chemical. Your food gets a nice squeeze from the upper part of the stomach (the fundus) and then your stomach churns like a washing machine to break food down and form chyme.
Chemical digestion happens through the secretions that are released in the stomach, including:
Stomach acid: destroys microorganism and breaks down proteins and plant structure
Pepin: an enzyme that breaks down proteins
Intrinsic factor: binds to B12 to help with absorption in the small intestine
Gastrin: a hormone that helps stimulate movement and the release of stomach acid
All sounds pretty complex, right? That means there are many areas where things can go wrong.
What’s your poop personality? Find out here!
And this is where GERD (gastroesophageal reflux disease) comes in, which impacts around 18.1-27.8% of North Americans (PMID: 30228725). This is where stomach contents reflux, or move back, through the esophagus, which then leads to symptoms and/or complications. The most common symptom is heartburn, and other symptoms include regurgitation, chest pain, hoarseness, throat clearing, and chronic cough.
Those with GERD will either be categorized as NERD, meaning no damage is present in the esophagus, or as erosive reflux disease, meaning that there is inflammation, erosion, or thickening of cells in the esophageal tissue. Erosive reflux disease is the most severe, because the damage of tissue can lead to thickening (Barrett’s esophagus), which can then lead to esophageal cancer.
Symptoms in those with NERD are thought to be caused by hypersensitivity of the tissue versus actual damage to the tissue, when exposed to stomach contents (the refluxate).
So what causes GERD to begin with?
The most common cause is a poorly functioning lower esophageal sphincter (LES). Simply put, the door that should be closed after food enters the stomach, stays open to some degree. This allows the refluxate (acid, bile acids, pepsin, food contents, and microbes) to move into the esophagus and cause damage and/or symptoms.
The LES becomes more relaxed (aka open), due to reduced strength or pressure of the muscles surrounding it, increased stomach pressure, or the presence of a hiatal hernia (when the stomach pushes up through the esophagus leaving the door open). Dysfunction of the sphincter can be caused by medications and tobacco use, and reduced pressure of the muscles can be caused by alcohol, coffee, chocolate, peppermint, onions, garlic, fats, and spicy foods.
Gastric pressure can be caused by slowed stomach emptying (gastroparesis or nerve damage), eating too quickly or too much in one sitting, gas (air swallowing or gas production), and tight clothes or pressure on the abdomen.
Another cause of GERD is esophageal hypersensitivity, which is the major cause of symptoms in NERD. The tissue in the esophagus lacks mucus-secreting cells and bicarbonate production, so it has no way to neutralize stomach acid when exposed. Exposure can lead to cell damage, which then causes more hypersensitivity of the nerves in the tissue, which means they are more prone to damage (erosive disease) or reaction to the refluxate to cause symptoms (NERD).
This is also a theory that exposure to infection, through foodborne illness or h.pylori, may lead to hypersensivity of tissue, as well as dysfunction with the LES and gastric emptying. This has yet to be proven.
In addition to the above, another common cause that is poorly defined in research are disordered eating behaviors and eating disorders. The act of binging or purging cycles can lead to more damage in the esophagus and dysfunction of both the LES and stomach. And under-nutrition, as well as weight loss, will slow gastric emptying and increase gastric pressure. This can typically improve with weight restoration, but may not always be fully back to “normal” in severe cases.
So what actually causes symptoms, then?
If you have GERD, you already more prone to symptoms, so the foods listed above that lower LES pressure, as well as anything that increases gastric pressure, will lead to more symptoms. In addition to those, you may experience symptoms with acidic foods, as they interact with the tissue in the eosphagus.
Stress also plays as role as it reduces stomach acid secretion and reduces gut motility, which leads to slowed stomach emptying and increased gastric pressure. Poor posture while eating, as well as tight clothes or pressure on your abdomen can all also trigger symptoms by increasing gastric pressure or reducing the LES pressure.
What now?
If you’re experiencing symptoms, it can be helpful to see a gastroenterologist for testing and assessment. Communicate your history and the different pieces that connect for you and may be involved in your “cause.” If you’ve been diagnosed, it is helpful to understand if you’re in the NERD or erosive reflux disease category, which can be tested through both an endoscopy and a reflux monitoring test. Discuss this with your doctor, as your treatment may be tailored to that category.
If you are looking for more support for your GERD, outside of the medical management you currently have with your doctor, our team of specialized dietitians may be able to help. Learn more about what we do here!
Are you frustrated with your IBS symptoms? Do you desire to be confident in your food choices? Do you want to have a healthier relationship with your body and diet? Are you ready to take control of your IBS?
Guides: